Can diabetes tech save patients time? Maybe, but I actually hope it doesn’t
By Alicia Shelly, MD, FACP
6 min read

Because managing diabetes effectively can be a major time commitment, many of my patients look for ways to save themselves time each day. More and more, patients ask me if tech may be able to help.
I understand where they’re coming from. Our shared goal is diabetes management, and time is the currency patients spend to try to achieve it.
But when a patient asks me if a continuous glucose monitor (CGM), connected insulin pen, or other piece of diabetes tech will save them time on a day-to-day basis, I can’t really guarantee that. And that may be a good thing.
The possible time-adding paradox of CGMs
Let’s consider a hypothetical patient switching from a blood glucose monitor (BGM) to a CGM. Each time they sync their CGM with their smartphone to check their blood sugar, that single task may be quicker than pricking their finger and using a test strip. But that’s not the full picture.
One survey revealed that adults with type 2 diabetes who started using CGMs checked their glucose more frequently than prior to using a CGM.1 So if a patient with type 2 diabetes moves from doing 1 finger stick per day to checking their glucose 5 times a day with a CGM, they may actually be spending more time checking their glucose than they did with a BGM.
As their health care provider, I know those extra checks and extra time may help to strengthen their self-management. Many of my patients tell me they value the increased awareness of their blood sugar throughout the day. And I’ve found that even if my patients end up spending more time monitoring when they adopt a CGM, it doesn’t tend to bother them as long as they perceive it as a convenience.
In that same survey, most people also felt that using the CGM fit well enough within their lifestyle.1
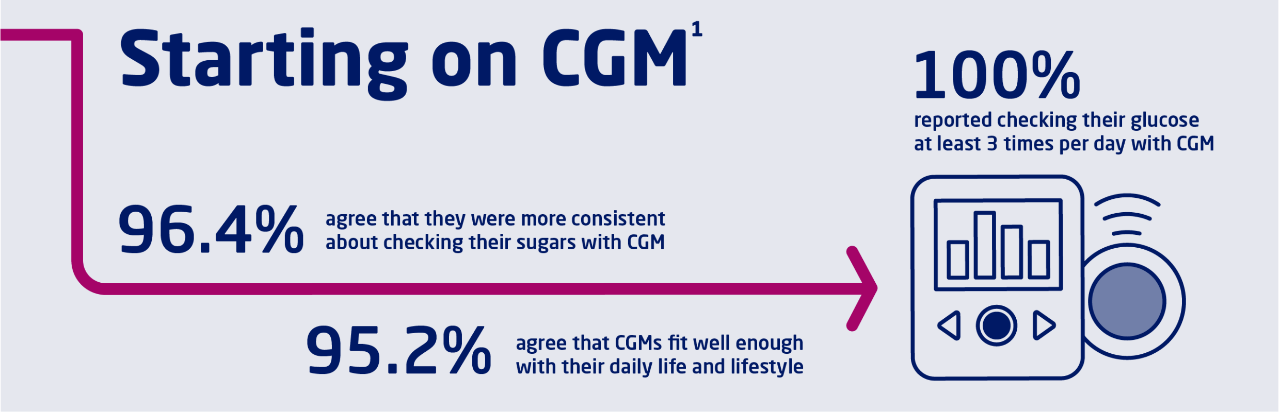
In a 2022 survey of adults with type 2 diabetes who started using CGMs in the past 12 months1:
96.4% agree that they were more consistent about checking their sugars with CGM
95.2% agree that CGMs fit well enough with their daily life and lifestyle
100% reported checking their glucose at least 3 times per day with CGM
Study design:
Mixed qualitative and quantitative survey-based study of 84 adults with type 2 diabetes who started using a CGM for the first time within the previous 12 months to evaluate experience and impact of CGM.
This is consistent with my experience as a clinician. In fact, many of my patients who have started using or have switched to CGMs tell me they feel like they’re saving time. That may or may not be the case, but I don’t see a need to put a stopwatch on them. For me, the key is that my patients are engaged and feel good about their self-management plan.
Helping patients make the most of their diabetes management time? There’s an app for that
CGMs aren’t the only piece of diabetes tech that could encourage patients to spend time managing their diabetes. My patients who use diabetes management apps often tell me that the apps feel like time-savers as well. If they sync their CGM, smart pen, or smart pump compatible apps, it can create a log of their insulin doses and glucose levels for them, potentially removing the added responsibility of carrying a notebook.2
Keeping their dose history and glucose data in an app may help patients see the full picture.3 I usually suggest to my patients that they review their diabetes data in the app between visits. Although I’m asking them to spend more time on the app than they would have with their logbook, the app may facilitate their learning about the relationship between their insulin dose and glucose levels. I’ve had patients tell me they like getting that kind of insight from their app.
Some of my patients use diabetes apps to help them self-manage more independently, such as calculating bolus insulin doses at mealtimes.3 In my view, apps do help save these patients time by enabling them to adapt their routine and make decisions in the moment.

Many of my patients who have switched to CGMs tell me they feel like they’re saving time. That may or may not be the case, but I don’t see a need to put a stopwatch on them.
Spending time where it matters most through telehealth and texting
Telehealth is another type of tech that can help patients who value saving time, even if they may end up spending more time communicating with me in the long run.
Many of my patients tell me they prefer virtual visits for the time they save driving to our practice or sitting in our waiting room.4 Accessing information through our patient portal has helped save patients time that they might otherwise have spent on the phone or digging through their files. Online billing lets them make payments before appointments instead of calling or waiting at the reception desk. The portal gives them another channel for timely sharing of data from their diabetes apps, too.
And I’ve found that because we can usually make virtual visits fit with patients’ schedules, they tend to keep appointments more consistently, which helps them stay engaged with their care.
Since many patients prefer (or are limited to) using mobile phones, my team also sends text messages to provide reminders about appointments, prescription refills, and check-ins to see if patients need to talk about anything. We allow patients to text us too—for a patient who’s pressed for time, being able to text their question to my staff or a diabetes educator can mean a lot.4
When you add it all up, the time my patients save by not commuting to my office may be offset by how much more frequently they stay in contact. But to me, that’s the point. If my patient is more engaged with their care, any extra time is being put to good use.

To help optimize their use of diabetes technology management, patients need support
CGMs, apps, and telehealth may help make some aspects of diabetes management more efficient, but tech by itself can’t solve people’s time-management challenges. Patients still need help from their care team.
Let’s say I tell a patient that a diabetes device may help them optimize their time, but I don’t provide any guidance or support for using it. They may spend hours trying to figure it out and end up feeling frustrated and possibly giving up. I might inadvertently have made them lose trust in my recommendation or lose confidence in themselves.
Support has to start before they use the tech and be available when they need it. I start by asking about their priorities and making sure I recommend tech that’s suited to their individual needs. I also try to help patients set expectations and break down the process of tech adoption into specific, manageable steps or goals.
I tell my patients that the door is always open for them to ask questions of my staff and myself. Whenever possible, I also help them find other resources such as group classes with a diabetes care and education specialist. If they’re struggling, whether it’s with tech or time management, my team is here to help.
Tech-up Follow-ups
- Ask your patients who struggle with diabetes self-management which tasks are taking up most of their time.
- Show them how a particular digital health tool works and ask them to compare it to the time they spend on the corresponding non-tech task.
- Encourage them to give a new digital health tool a try for at least 2 weeks to experience the potential time savings for themselves.

Alicia Shelly, MD, FACP
Douglasville, Georgia
Dr Shelly is a primary care provider who regularly sees patients with diabetes. She is a board-certified internal medicine physician at Wellstar Primary Care in Douglasville, Georgia.
Alicia Shelly received a fee from Novo Nordisk for her participation.
–— Recommended for you –—
References
- Johnston AR, Poll JB, Hays EM, Jones CW. Perceived impact of continuous glucose monitor use on quality of life and self-care for patients with type 2 diabetes. J Deman. 2022;6. doi:10.1016/j.deman.2022.100068
- Islam SMS, Mishra V, Siddiqui MU, et al. Smartphone apps for diabetes medication adherence: systematic review. JMIR Diabetes. 2022;7(2):e33264. doi:10.2196/33264
- Fu H, Wyman J, Peden-McAlpine C, Draucker C, Schleyer T, Adam T. App design features important for diabetes self-management as determined by the self-determination theory on motivation: content analysis of survey responses from adults requiring insulin therapy. JMIR Diabetes. 2023;8:e38592. doi:10.2196/38592
- Ashrafzadeh S, Hamdy O. Patient-driven diabetes care of the future in the technology era. Cell Metab. 2019;29(3):564-575. doi:10.1016/j.cmet.2018.09.005
The Diabetes Tech-upTM Podcast
Join our expert cohosts for a series of discussions about how they’re integrating diabetes tech with patient-centered care to help optimize diabetes management.
The Mission of Diabetes Tech-upTM
Diabetes Tech-upTM is sponsored by Novo Nordisk, a global leader in diabetes. We believe that adoption of innovative technologies can help appropriate patients better manage diabetes. Our goal is to provide information to help health care professionals on the front line of diabetes care strengthen their understanding of diabetes technologies and implement them where they can have the greatest impact.




Share: