How can we build on A1C? Looking at metrics that can help with daily glycemic control
By Amy Hess-Fischl, MS, RDN, LDN, BC-ADM, CDCES and Amy Tenderich, MA
10 min read

For nearly 50 years, the hemoglobin A1C test has been the go-to metric for evaluating glycemic management.1 But with wearable diabetes tech like continuous glucose monitors (CGMs) becoming more mainstream, patients and providers no longer have to wait months until the next A1C test to see how well their diabetes management plan is working. There are a lot of newer tech-enabled metrics that patients and providers can use to help inform their diabetes management decisions.
What metrics, in addition to A1C testing, can people look at to engage with their diabetes management? How can providers help their patients understand this data? To explore these questions and more, we talked with Amy Tenderich, a technology journalist and prominent patient advocate who lives with type 1 diabetes, and Amy Hess-Fischl, an award-winning diabetes care and education specialist. Amy Tenderich and Amy Hess-Fischl both received a fee from Novo Nordisk for their participation.
Before we talk about some of the other metrics also being used today, let’s talk about A1C. How useful is it for patients and providers?

Amy Tenderich
Well, the A1C test is still helpful in that it gives you an average measure of your blood glucose levels over the past 2 to 3 months.2 It’s still the most recognized metric in clinical settings to assess glycemic control,3 and it’s a simple way to evaluate the clinical trial results of different diabetes therapies at a high level.4
But here’s the thing about averages: they’re more useful when you’re considering long-term trends. I personally don’t go more than 20 minutes at a time without thinking about my diabetes. In any of those individual moments, I don’t always think about my 3-month average. I think about my present, about how I’m feeling and what my glucose levels are right now. I might average 60 miles an hour on the freeway, but if I were to hit 100 miles an hour, there could be consequences. I need both the long-term and short-term trends to know how I’m truly doing with my diabetes management.
Fortunately, there are other metrics now that will tell me how my glucose levels are doing on a day-to-day basis, and a lot of them are enabled by my CGM.

Amy Hess-Fischl
As a provider, an A1C test is a useful metric for me to quickly gauge how a patient is doing overall. I can’t envision a world anytime soon where it gets replaced. Like Amy T said, it’s still the primary metric used for making decisions on overall glucose management and assessing the risk of long-term complications associated with diabetes. That’s on a global scale, too—there are many communities in other parts of the world where CGM adoption has been relatively low, and therefore won’t have access to CGM-enabled metrics.2,5
It is also worth noting that measurements like time-in-range (TIR), time-below-range (TBR), time-above-range (TAR), and the glucose management indicator (GMI) are recognized as useful in clinical settings by the American Diabetes Association because they may provide insights for a more personalized diabetes management plan.6 The target "range" for TIR is between 70-180 mg/dL for many patients with type 1 or type 2 diabetes, and when patients spend 70% of their time there, that correlates to an A1C of about 7%.7

I think the A1C feels like an exam you can often fail without understanding why. TIR is useful in the immediate term and can be easy to understand for those of us living with this condition.
So, A1C is still a useful big-picture metric, and we now have other ways to evaluate and course correct glycemic management between A1C tests.
Still, as a provider, I do recognize that the A1C test can feel challenging for patients. I’ve seen how people can attach a lot of emotion to the numbers they see, and when you look at the data from the T1D exchange in 2016-2018, many children, adolescents, and adults did not achieve an A1C goal <7.5%.8 So when I’m working with patients, it’s my job to deconstruct those numbers for each person to see how we can move the needle.
And, now that we have access to them through newer technology, I can't help but want to layer on additional metrics that can help me and my patients get a clearer picture of how they are doing with their glucose levels day to day and even hour to hour.
OK, let’s talk about some of those other metrics. Which newer diabetes metrics can help people engage with their daily management?

Amy Tenderich
Within the patient community, there has been a big push, known as the Beyond A1C movement, to drive awareness and adoption of TIR as a key tool for assessing glycemic control each day. TIR is just one of several metrics included on the ambulatory glucose profile (AGP) report.9 In contrast to A1C results, looking at TIR data from an AGP report can help offer people with diabetes actionable insights into the changes in their glucose levels moment to moment.7 I think the A1C feels like an exam you can often fail without understanding why. TIR is useful in the immediate term and can be easy to understand for those of us living with this condition.
Again, this is possible thanks to the proliferation of CGMs, and that’s given the movement a lot of momentum in recent years. Someone wearing a CGM can essentially check their glucose in real time, either on their device or in a compatible app on their phone.10 People can see for themselves which way they’re trending and what percentage of time they’re staying within their target blood glucose range.
When you’re able to look at your glucose that way, on your own or with your provider, it allows you to ask questions like, “What can I work on to get into that target range more consistently?” For me, I might look at the app that my CGM connects to and say, “Wow, my TIR is better on Tuesdays and Thursdays, what’s going on there? Oh, right, those are the days when I work out.”
My provider and I periodically go over this report together, trying to map changes in my routine to fluctuations in my data so we can decide together what the best response might be. I recommend that everyone wearing a CGM does this with their provider.
Something to talk about
Start an open, helpful dialogue using data from a patient’s CGM.

Terri
Diabetes type: T2D
A1C for January 18-April 18: 7.5%
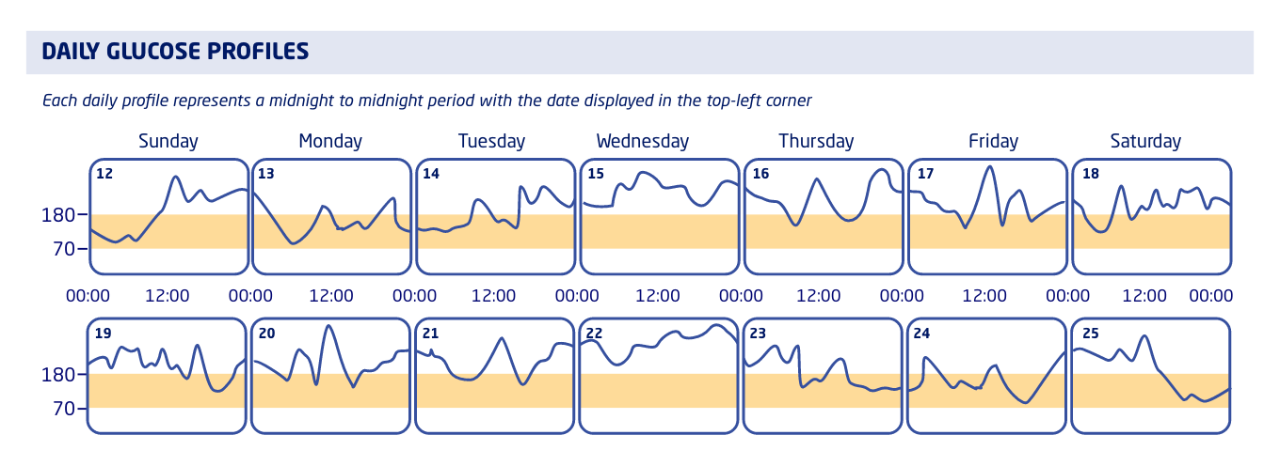
Each daily profile represents a midnight to midnight period with the date displayed in the top-left corner
Notes: Even though Terri’s 3-month A1C is not excessively high, we looked at her AGP from the week of March 12-25. For several days in a row, her glucose levels were outside of her target range for more time than usual.
Ask Terri:
- Can you recall how this particular week went for you?
- Can you tell me about what you did and what you ate on those days?
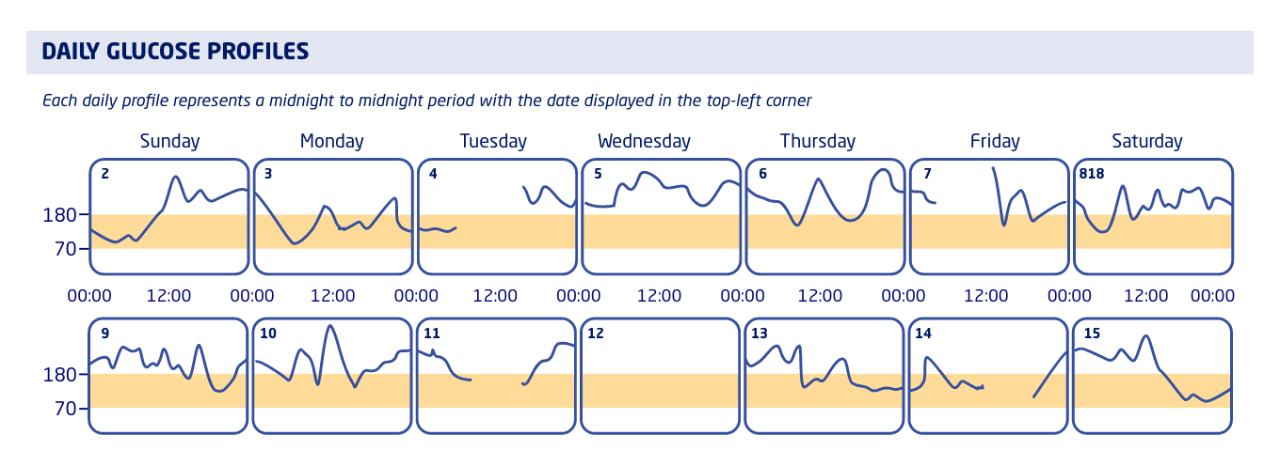
Each daily profile represents a midnight to midnight period with the date displayed in the top-left corner
Notes: We noticed missing data during the day on Tuesdays and Fridays in early April, as well as one completely blank day on April 12. Looks like Terri wasn’t wearing her CGM during those times.
Ask Terri:
- It looks like we have some missing data on a few days last month. Can you tell me more about that?
- What would help you wear your CGM more consistently?

Amy Hess-Fischl
I love me some AGP. The AGP is a one-page report that summarizes the last 14-90 days, depending on the time frame chosen, of a person’s glucose data.9,11 It’s a great tool to have on hand when giving someone a snapshot about how their glucose management is going.
In addition to TIR, I can also sit down and talk through someone’s TAR or TBR. Amy T, I think what’s great about your example with your workout days is that it shows how empowering it can be to have this data on hand. For people who are consistently hitting their target range, we can identify and reinforce good habits. If someone is having trouble staying in range, maybe our conversations will help them find a way to make an adjustment in their routine that pushes them closer to their goal. Again, it’s about moving the needle.
The AGP report also includes the GMI, which is calculated based on a person’s average glucose levels over that 14-, 30-, 60-, or 90-day period and tries to assess their glucose management on a broader scale. (We used to call this estimated A1C, or eA1C, but people found that name confusing.)11,12 In combination with the other metrics on the report, this is another way providers can try to identify trends in a person’s glycemic control.
Tech delivers: From detailed data come meaningful metrics11-14
(paired with CGM)
SELECTED METRICS YOU MAY FIND USEFUL
TIR, TAR, TBR
Measures the amount of time an individual’s blood glucose falls within, above, and below a person’s target glucose range (typically 70-180 mg/dL), respectively, usually over a period of 14, 30, 60, or 90 days. These measurements are expressed as percentages.
GMI
Uses an individual’s average glucose levels to estimate their A1C results based on a large sample of individuals with similar average glucose levels.
For the full list of standardized CGM metrics for clinical care, refer to Table 6.2 in the American Diabetes Association’s 2023 Standards of Care in Diabetes.
SELECTED FEATURES YOU MAY FIND USEFUL
Basal, bolus, and correction doses
Available connected pens can record the amount and timing of insulin doses. Insulin data is available as a downloadable report to be compared with data on glucose levels and food intake.
With access to technology rising, people with diabetes can have more data at their fingertips than ever. What should providers emphasize when recommending these devices to patients?

Amy Hess-Fischl
Whether we’re talking about the AGP report or any of these metrics that tech is letting us see more consistently, it’s important to level set—the data you get is only as good as that person’s device usage. An individual needs to be wearing a CGM for at least 70% of the time over 14 days to generate useful data.9
So yes, tech can help empower people to look at their data and do something about it, but first they have to be willing to wear the tech. I work with a lot of people with diabetes, type 1 and type 2, younger and older, who aren’t as engaged with their care as they could be. I think a lot of the time it’s because they don’t know how.
With my teenage and young adult patients in particular, a lot of them don’t want to wear a CGM all the time, so I have to negotiate. “Can we start with 2 weeks, just so we can look at the report and see what there is to see?” If that works, then they can get a taste of what tech has to offer.
And as providers, I think we owe it to ourselves to keep initiating these conversations. The more success we have educating people about tech and getting them interested enough to do a trial run, the better we will become at making those recommendations in the first place. When we find out what works and doesn’t work for some people, we can be quicker to recognize what might help someone else.

Amy Tenderich
It’s worth mentioning that while we’ve focused a lot on the data that CGMs can provide, there are some people who wear a smart insulin pump or use a connected insulin pen without a CGM. For those people, there’s still a lot of value in automatically logging their insulin doses and having that data at a glance. And actually, there are some people calling for the standardization of digital insulin data, which could yield something similar to the AGP report but for tracking insulin distribution.15
In general, I would say that capturing data in the previous era was a lot more haphazard. You got the reading from sticking your finger several times a day, and then you had to log all of that data and all of your insulin doses manually. Compare that to now where some devices have their own software that can generate a version of your AGP report on the fly.16
One CGM I like can send you a weekly TIR report, which is nice for offering reminders and reinforcement. It also has a feature that can tell me what my best day was in the last week, so I like to look at that and compare it to my calendar to see what I can carry over into my daily routine. That ability to reflect on my health habits and double down on what’s working is what I find really encouraging, and the tech makes that possible.

As providers, I think we owe it to ourselves to keep initiating these conversations. The more success we have educating people about tech and getting them interested enough to do a trial run, the better we will become at making those recommendations in the first place.
For people who are trying to become more engaged in their diabetes care, the breadth of available metrics can be overwhelming. What can providers do to help patients navigate their data?

Amy Hess-Fischl
The primary care providers I work with get about 15-20 minutes to talk to their patients. That’s not a lot of time to talk to someone about diabetes data, let alone other possible issues, so you have to make the most of it.
Each patient is different, so I try to make sure I am taking an individualized approach to every appointment. I know I could spend as little as 5 minutes digging into an AGP report, or I could spend upwards of 30 minutes, depending on how much time we have and what is important to them.
I would encourage my fellow providers to make it a habit of asking patients what they want to focus on. Then you can confidently sit down and say, “Let’s focus on TIR today—how do we address some of these spikes?”
Health care providers can help people with diabetes engage with their care by drawing connections between their data and their daily habits.10

Amy Tenderich
I think for patients to be better oriented with their data, providers also need to be prepared to engage with it. Not everyone gets to see an endocrinologist or a certified diabetes care and education specialist (CDCES) like Amy H. A 2021 survey of 303 health care providers showed that only 56% of primary care providers were aware of TIR, and only 67% were familiar with the standardized CGM metrics for clinical care.17
To Amy H’s point, the AGP report can definitely be a lot to get through, which is why some researchers have been working on a single number to summarize it. In 2022, a group of clinicians proposed a new metric called the glycemia risk index (GRI), which compares a person’s risk of hypo- and hyperglycemia and rates their overall management on a scale from 0-100.18
One of the points of this new measurement is that somebody can have good TIR but still too much TBR or TAR. So, we’ve been talking about going beyond A1C, but now some people are saying we should go beyond TIR. The GRI could make it simpler for providers to assess multiple CGM reports.18 It remains to be seen whether GRI will catch on, but it’s always encouraging to know that the diabetes community is continuing to push for better ways to talk to each other about diabetes.
Tech-up Follow-ups
- Ask your patients who are less engaged with their diabetes management what they need in order to better understand how they’re doing. Be prepared to recommend tech, like CGMs, connected pens, or AID systems to appropriate patients, which can provide those patients with timely insights.
- Prepare to talk about one metric, such as TIR, that can supplement discussion of your patients’ A1C results.
- Prepare some questions for your patients who are already wearing a CGM about what observations they’ve made based on their data and what changes they’ve made.

Amy Hess-Fischl, MS, RDN, LDN, BC-ADM, CDCES
Chicago, Illinois
Amy is a diabetes care and education specialist and registered dietitian who sees type 1 and type 2 diabetes patients daily. She oversees their education recognition program and coordinates the Teen and Adolescent Diabetes Transition Program at University of Chicago’s Kovler Diabetes Center. She received the American Diabetes Association’s Outstanding Educator of the Year award in 2022.

Amy Tenderich, MA
Santa Barbara, California
Amy is a journalist, nationally known patient advocate, and diabetes tech expert. She was the founder and editor of DiabetesMine.com and former Editorial Director of Diabetes & Patient Advocacy at Healthline Media. She organizes and hosts the biannual DiabetesMine Innovation Forums (Innovation Summit, D-Data ExChange) that connect patient and industry leaders. Amy also lives with diabetes, having been diagnosed with type 1 diabetes in 2003.
Both contributors received a fee from Novo Nordisk for their participation.
–— Recommended for you –—

ARTICLE
Creating "aha!" moments: 3 ways I use diabetes tech to help patients overcome self-management barriers
Get tips for using diabetes data to help patients build knowledge, discover motivation, and draw connections between their actions and their glucose levels.
By Alicia Shelly, MD, FACP | 6 min read
References
- John WG, Mosca A, Weykamp C, Goodall I. HbA1c Standardisation: history, science and politics. Clin Biochem Rev. 2007;28(4):163-168.
- Eyth E, Naik R. Hemoglobin A1C. StatPearls Publishing; 2023. Updated March 13, 2023. Accessed August 2023. https://www.ncbi.nlm.nih.gov/books/NBK549816/?report=printable
- Wright LA, Hirsch IB. Metrics beyond hemoglobin A1C in diabetes management: time in range, hypoglycemia, and other parameters. Diabetes Technol Ther. 2017;19(S2):S16-S26. doi:10.1089/dia.2017.0029
- Lipska KJ, Krumholz HM. Is hemoglobin A1c the right outcome for studies of diabetes? JAMA. 2017;317(10):1017-1018. doi:10.1001/jama.2017.0029
- Graham C. Continuous glucose monitoring and global reimbursement: an update. Diabetes Technol Ther. 2017;19(S3):S60-S66. doi:10.1089/dia.2017.0096
- ElSayed NA, Aleppo G, Aroda VR, et al, on behalf of the American Diabetes Association. 6. Glycemic targets: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S97-S110. doi:10.2337/dc23-S006
- Beck RW, Bergenstal RM. Beyond A1C-standardization of continuous glucose monitoring reporting: why it is needed and how it continues to evolve. Diabetes Spectr. 2021;34(2):102-108. doi:10.2337/ds20-0090
- Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016-2018. Diabetes Technol Ther. 2019;21(2):66-72. doi:10.1089/dia.2018.0384
- Kröger J, Reichel A, Siegmund T, Ziegler R. Clinical recommendations for the use of the ambulatory glucose profile in diabetes care. J Diabetes Sci Technol. 2020;14(3):586-594. doi:10.1177/1932296819883032
- Arbiter B, Look H, McComb L, Snider C. Why download data: the benefits and challenges of more diabetes data. Diabetes Spectr. 2019;32(3):221-225. doi:10.2337/ds18-0099
- Czupryniak L, Dzida G, Fichna P, et al. Ambulatory glucose profile (AGP) report in daily care of patients with diabetes: practical tips and recommendations. Diabetes Ther. 2022;13(4):811-821. doi:10.1007/s13300-022-01229-9
- Bergenstal RM, Beck RW, Close KL, et al. Glucose management indicator (GMI): a new term for estimating A1C from continuous glucose monitoring. Diabetes Care. 2018;41(11):2275-2280. doi:10.2337/dc18-1581
- Association of Diabetes Care and Education Specialists, APhA. Personal Continuous Glucose Monitoring Implementation Playbook. 2020. Accessed August 2023. https://www.diabeteseducator.org/practice/practice-tools/app-resources/professional-cgm-playbook
- Sy SL, Munshi MM, Toschi E. Can smart pens help improve diabetes management? J Diabetes Sci Technol. 2022;16(3):628-634. doi:10.1177/1932296820965600
- Wolpert H, Polonsky WH, Rodbard D. Insulin metrics: need for development of consensus standards for reporting of insulin dosing data. Diabetes Technol Ther. 2021;23(7)522-526. doi:10.1089/dia.2020.0631
- Doyle-Delgado K, Chamberlain JJ. Use of diabetes-related applications and digital health tools by people with diabetes and their health care providers. Clin Diabetes. 2020;38(5):449-461. doi:10.2337/cd20-0046
- Kenney J, Tait J, Briskin A, et al. Awareness of time in range varies by type of health care provider. The diaTribe Foundation. 2021. Accessed October 2023. https://diatribe.org/sites/default/files/ADA%20Posters%20%E2%80%93%20Awareness%2C%20v4.pdf
- Klonoff DC, et al. A glycemia risk index (GRI) of hypoglycemia and hyperglycemia for continuous glucose monitoring validated by clinician ratings. J Diabetes Sci Technol. 2022:19322968221085273. doi:10.1177/19322968221085273
The Diabetes Tech-upTM Podcast
Join our expert cohosts for a series of discussions about how they’re integrating diabetes tech with patient-centered care to help optimize diabetes management.
The Mission of Diabetes Tech-upTM
Diabetes Tech-upTM is sponsored by Novo Nordisk, a global leader in diabetes. We believe that adoption of innovative technologies can help appropriate patients better manage diabetes. Our goal is to provide information to help health care professionals on the front line of diabetes care strengthen their understanding of diabetes technologies and implement them where they can have the greatest impact.



Share: