Creating “aha!” moments: 3 ways I use diabetes tech to help patients overcome self-management barriers
By Alicia Shelly, MD, FACP
6 min read

Some of my peers in internal medicine tell me they think prescribing continuous glucose monitors (CGMs) for their patients with diabetes isn’t worth the trouble. They think the learning curve will be too steep, or that their patients won’t use the device. Sometimes they point to issues with insurance coverage as the main reason they don’t consider it.1
I think they don’t know what they’re missing.
I’ve been prescribing CGMs for several years now—in my experience, the learning curve has started to flatten out due to design changes, and many of my patients are more willing to try new tech. Medicare has updated their CGM coverage criteria to make more patients with type 2 diabetes eligible, there are online CGM coverage calculators which let providers and patients check commercial coverage in minutes, and patient assistance programs may help with out-of-pocket costs.2,3
But in my opinion, one of the main reasons to consider CGMs (or any diabetes data-capture technology) is the insight that we and our patients can potentially harness from the data it provides.4
Here are examples of 3 ways that diabetes technology has helped my patients make progress in their diabetes management, plus a potential key to helping them sustain that progress on their own.
1. Looking at diabetes data together helps pinpoint where change may be needed4
I love seeing the lightbulb go on over a patient’s head—that moment when they gain a better understanding of glucose management that empowers them to take action. In my experience, some people have their “aha!” moment when they compare how they perceive their glucose levels with a more objective point of view. I help them see it clearly with blood glucose data from diabetes devices.
One of my patients with type 2 diabetes felt confident he had his glucose under control. He was administering multiple daily injections of insulin and said he felt fine, but his A1C was higher than I expected. He assured me that he didn’t need a CGM.
When I asked him how he’d feel about wearing one on a 2-week trial basis, he was suddenly more receptive to the idea.
Two weeks later, the ambulatory glucose profile (AGP) report generated from his CGM data showed a very different picture than what he was expecting. While he wore the CGM, he had spent nearly 80% of his time outside of his target glucose range. He was shocked.
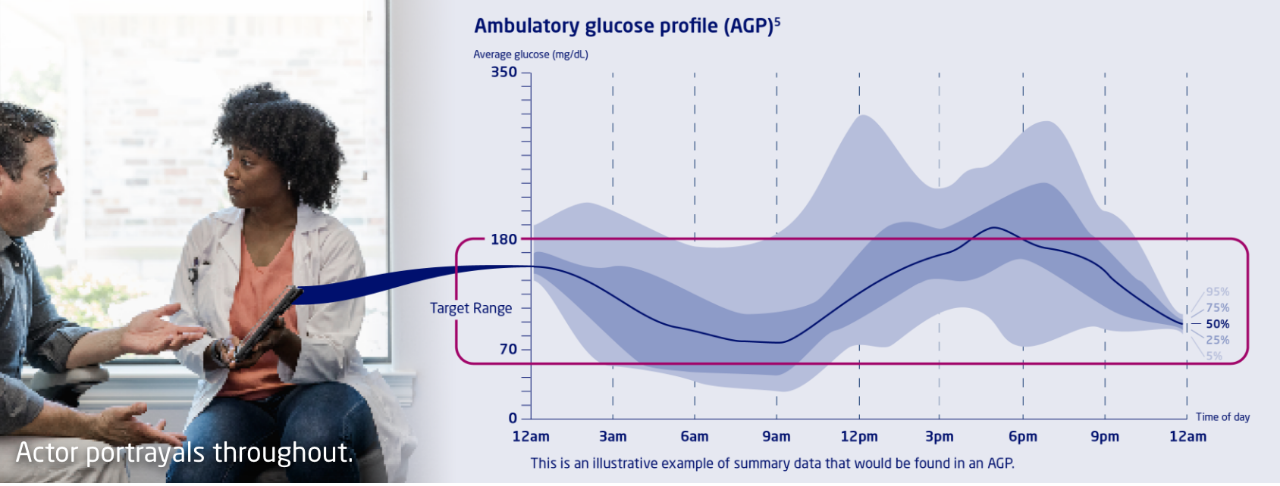
Looking at your patients’ AGP together may help them see where they can make changes to their self-management routine.
We looked at the graph together and I asked him to revisit his actions at certain times of the day. He started making the connection. He remembered when he took his insulin (and when he didn’t), when and how much he had exercised, and what he had eaten. He saw the ways his actions had corresponded with his roller coaster of low and elevated glucose.
His eyes had been opened, and he was ready to talk about specific things he could do differently.
2. Talking tech can uncover knowledge gaps and health literacy barriers
Situations like the above are why I ask open-ended questions. If I had let the conversation drop when the patient told me he felt fine, I wouldn’t have learned what was behind his hesitation to try a CGM. When I invited him to explain, he told me that he didn’t want to commit to wearing a device for the long term.
That led me to mention the trial period, and the conversational roadblock lifted. I’d presented an option he didn’t know he had. The barrier wasn’t the tech itself—it was the commitment.

I love seeing the lightbulb go on over a patient’s head—that moment when they gain a better understanding of glucose management that empowers them to take action.
I take this approach any time I discuss diabetes technology. I treat people at all levels of health literacy, and sometimes people don’t know what they don’t know. When I ask open-ended questions and leave plenty of room for patients to answer, it helps me meet them where they are.
I had one patient who refused to consider injectable GLP-1 receptor agonist medications simply because they were injectable. At first, I assumed she didn’t like needles, but as we talked further, I realized she had the misconception that all injectable diabetes medicines were insulin. This discovery cleared the way for a much more productive conversation.
As a provider, I get plenty of “aha!” moments too.

Every patient has their own source of motivation—you can help them identify and act on it.
3. Using data from diabetes tech to help patients find motivation6
I’ve noticed that a feeling of progress can be motivating to people with diabetes. Whenever I can, I try to use diabetes tech and data to help illustrate how they’re changing their own story.
When a patient is struggling, I ask them why it’s important to them to manage their diabetes. Many patients tell me they want to have more time with their families or be able to enjoy a more active lifestyle. I point out that consistently managing their glucose levels might help with their long-term health, which is part of the bigger picture of their goal.7 For some of my patients, starting to use a CGM is a symbol of their progress, a visible commitment to reaching their goals.
Sometimes my patients and I review diabetes data to help illustrate what they’ve accomplished, like looking at current and old AGP reports side by side. I’ve noticed that even minimal changes in data may help them see that their efforts are worthwhile. I ask them what they think and how they feel about continuing their improved behavior or making further changes.
As we talk, if I can see that they feel a renewed sense of commitment, I usually try to help the person set a specific, manageable goal that may help them move forward—for example, setting a goal to stay within their target range for a full day, from breakfast to bedtime. If they achieve their goal, it may help reinforce their belief that they have the skills and the tools to sustain their momentum.6
Bridging the gap with training and support options8,9
I think the key to surmounting the learning curve is finding the right learning experience for each patient. Some of my patients are hands-on learners. Just explaining how a device or app works doesn’t help them absorb the knowledge in a way that’s useful. But when one of my nurses demonstrates it and lets the patient try it themselves, I see their eyes light up. For these people, it may also help to watch how-to videos while they have the device in hand.
I know some patients who prefer social interactions and tend to learn well in group settings. For these people, I like to refer them to classes with a certified diabetes care and education specialist (CDCES). These classes allow patients to learn in two ways: from listening to the CDCES and from interacting with their fellow patients.
If a patient is struggling with their device, I gently prompt them to describe how they’re using it. That lets them show me how much they know and helps me identify any knowledge gaps I may need to fill. I’m careful with my tone—I don’t want anyone to feel embarrassed or reprimanded. I try to let them strengthen their knowledge and skills at their own pace. If we do our best to figure it out together, and they’re still not feeling it, it’s possible that tech might not be right for them. And that’s OK.
With every patient, I ask what their goals are, and how I can help them get there. If I feel diabetes technology may be appropriate, I present it as an option. And if the person grasps how using a digital tool may put them on the path toward their goals, then we proceed.
Tech-up Follow-ups
- Identify 1 or 2 patients who have challenges with their diabetes self-management routine.
- Prepare a few open-ended questions that might help them express why they may be struggling.
- Consider what kind of tech might be able to help them. Describe it to the patients and listen to how they respond.

Alicia Shelly, MD, FACP
Douglasville, Georgia
Dr Shelly is a primary care provider who regularly sees patients with diabetes. She is a board-certified internal medicine physician at Wellstar Primary Care in Douglasville, Georgia.
Alicia Shelly received a fee from Novo Nordisk for her participation.
References
- Lanning M, Tanenbaum M, Wong J, Hood K. Barriers to Continuous Glucose Monitoring in People With Type 1 Diabetes: Clinician Perspectives. Diabetes Spectr. 2020;33(4):324–330. doi:10.2337/ds19-0039
- Moreau D. Final Medicare Continuous Glucose Monitor (CGM) Policy Goes Into Effect April 16th. Association of Diabetes Care and Education Specialists. April 7, 2023. https://www.diabeteseducator.org/danatech/latest-news/danatech-latest-news/2023/04/07/final-medicare-continuous-glucose-monitor-(cgm)-policy-goes-into-effect-april-16th
- Association of Diabetes Care and Education Specialists. CGM Insurance Coverage Tool from danatech. Accessed July 2023. https://danatech.policyacumen.health/
- Arbiter B, Look H, McComb L, Snider C. Why Download Data: The Benefits and Challenges of More Diabetes Data. Diabetes Spectr. 2019;32(3):221-225. doi:10.2337/ds18-0099
- Battelino T, Danne T, Bergenstal R, et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care. 2019;42(8):1593-1603. doi:10.2337/dci19-0028
- Rawlett K. Journey from Self-Efficacy to Empowerment. Health Care. 2014;2(1):1-9. doi:10.12966/hc.02.01.2014
- Association of Diabetes Care and Education Specialists, APhA. Personal Continuous Glucose Monitoring Implementation Playbook. 2020. Accessed July 2023. https://www.diabeteseducator.org/practice/practice-tools/app-resources/professional-cgm-playbook
- Swanson V, Maltinsky W. Motivational and behaviour change approaches for improving diabetes management. Pract Diabetes Int. 2019;36(4):121-125. doi:10.1002/pdi.2229
- Greenwood DA, Howell F, Scher L, et al. A Framework for Optimizing Technology-Enabled Diabetes and Cardiometabolic Care and Education: The Role of the Diabetes Care and Education Specialist. Diabetes Educ. 2020 Aug;46(4):315-322. doi:10.1177/0145721720935125
The Diabetes Tech-upTM Podcast
Join our expert cohosts for a series of discussions about how they’re integrating diabetes tech with patient-centered care to help optimize diabetes management.
The Mission of Diabetes Tech-upTM
Diabetes Tech-upTM is sponsored by Novo Nordisk, a global leader in diabetes. We believe that adoption of innovative technologies can help appropriate patients better manage diabetes. Our goal is to provide information to help health care professionals on the front line of diabetes care strengthen their understanding of diabetes technologies and implement them where they can have the greatest impact.




Share: